Learn more: PMC Disclaimer | PMC Copyright Notice
Impact of Windows and Daylight Exposure on Overall Health and Sleep Quality of Office Workers: A Case-Control Pilot Study
Abstract
Study Objective:
This research examined the impact of daylight exposure on the health of office workers from the perspective of subjective well-being and sleep quality as well as actigraphy measures of light exposure, activity, and sleep-wake patterns.
Methods:
Participants (N = 49) included 27 workers working in windowless environments and 22 comparable workers in workplaces with significantly more daylight. Windowless environment is defined as one without any windows or one where workstations were far away from windows and without any exposure to daylight. Well-being of the office workers was measured by Short Form-36 (SF-36), while sleep quality was measured by Pittsburgh Sleep Quality Index (PSQI). In addition, a subset of participants (N = 21; 10 workers in windowless environments and 11 workers in workplaces with windows) had actigraphy recordings to measure light exposure, activity, and sleep-wake patterns.
Results:
Workers in windowless environments reported poorer scores than their counterparts on two SF-36 dimensions—role limitation due to physical problems and vitality—as well as poorer overall sleep quality from the global PSQI score and the sleep disturbances component of the PSQI. Compared to the group without windows, workers with windows at the workplace had more light exposure during the workweek, a trend toward more physical activity, and longer sleep duration as measured by actigraphy.
Conclusions:
We suggest that architectural design of office environments should place more emphasis on sufficient daylight exposure of the workers in order to promote office workers' health and well-being.
Citation:
Boubekri M, Cheung IN, Reid KJ, Wang CH, Zee PC. Impact of windows and daylight exposure on overall health and sleep quality of office workers: a case-control pilot study. J Clin Sleep Med 2014;10(6):603-611.
Since the sick building syndrome of the 1970s and the World Health Organization's Declaration on Occupational Health for All in 1994,1 occupational health has become a salient issue among health professionals and architects alike. With the increased interest today in green architecture, daylighting is becoming an important design consideration. Typically, daylighting recommendations are made in the form of daylight factor levels ranging between 2% to 6% depending on building types and activities. A daylight factor is a percentage of indoor illuminance compared to the outdoor illuminance on a horizontal surface. The daylight factor principle is valid for stable overcast sky conditions only; sunny conditions are too dynamic and changing to be considered.
Although there are many studies that have explored the relationship between daylighting, psychological well-being, and workers' productivity or school children's performance,2–4 few have addressed the impact of daylight at the workplace on sleep, quality of life, and overall health. Exposure to light-dark patterns is one of the main environmental cues for circadian rhythms that influence approximately 24-hour biological, mental, and behavioral patterns such as sleep and activity.5 The timing of light exposure is very influential on these rhythms, and previous research has shown that office environment lighting during work hours can act as a regulator of circadian physiology and behavior, with blue-enriched artificial lighting even competing with natural light as an entrainer.6 Given that office hours occur during biologically natural daylight hours, we posit that light exposure in the office environment will have effects on sleep, and via sleep and other influences also have effects on physical and mental health.
There is much evidence that links insufficient sleep and/ or reduced sleep quality to a range of significant short-term impairments such as memory loss, slower psychomotor reflexes, and diminished attention.7–9 If windowless environments or lack of daylight affect office workers' sleep quality, there will be subsequent effects not only individually but also on a societal level, leading to more accidents, workplace errors, and decreased productivity. Sleep quality is also an important health indicator that may have effects on, and interactions with mood, cognitive performance, and health outcomes such as diabetes and other illnesses.10–13 Therefore, it is crucial to investigate the effects of daylight as it may provide a profound way to improve office workers' productivity and health as well as the safety of the community they work and live in. Deprivation to light damages monoamine neurons and produces a depressive behavioral phenotype in rats.14 In humans, a direct correlation between the severity level of seasonal affective disorder and exposure to natural light is well documented.15–17 Results of several studies suggest that both natural and artificial bright light, particularly in the morning, can improve significantly health outcomes such as depression, agitation, sleep, circadian rest-activity, and seasonal affective disorder.18–26
These effects of light exposure, or the lack thereof, illustrate the importance of proper light exposure for physical well-being and mental health. In our modern society, many responsibilities at the workplace and at home dictate self-imposed alterations and/or loss of daylight in our daily lives. Findings from the previously discussed research suggest that the light exposure determined by our daily schedules will have subsequent consequences on our mood, cognitive performance, and overall well-being. However, studies exploring the impact of daylight exposure, or the lack thereof, on the health of office workers are very scarce. Therefore, the aim of this study was to examine the influence of light exposure at the workplace, through the existence or absence of windows and of daylight, on office workers' sleep patterns, physical activity, and quality of life via actigraphy and subjective measures. In our study we compared two groups of office workers—those with windows and abundant levels of daylight and those without windows and with no direct contact with daylight at their workstations— in terms of overall health and well-being and subjective sleep quality using well-validated scales, and objective measures of sleep, activity levels, and light exposure via actigraphy. We hypothesized that office workers with windows in the work-place would have more light exposure, better sleep quality, more physical activity, and higher quality of life ratings compared to office workers without windows in the workplace.
METHODS
Participants
A total of 49 participants were recruited, including 27 day-shift workers in windowless workplaces and 22 comparable day-shift workers in workplaces with windows. Workers were selected from volunteers within administrative support staff and other office workers on the campus of the University of Illinois at Urbana-Champaign (UIUC) whose work schedule was from 08:00 to 17:00. The typical recruitment process was done by contacting an office manager, who in turn provided names of volunteers from his/her group. The participants were not told about the specific objectives of the study but were informed that the study was about the impact of workplace physical and social conditions on productivity and well-being.
In addition, a subset of the participants had actigraphy recordings to measure light exposure, activity, and sleep. A total of 21 participants had actigraphy recordings, including 10 office workers in windowless workplaces and 11 office workers in workplaces with windows. Participants were selected for actigraphy based on a convenience sample with volunteers from office locations with and without windows.
Once the volunteers were identified, daylight factors at their workstations were measured. Only daylight factors > 2% were kept in the study for workers in workplaces with windows. Generally, daylight factors < 2% are deemed not useful for task performance illumination. In this study, we define a windowless workplace as one without any windows or one where workstations were far away from windows and therefore had no exposure to daylight and no views to the outside world. The Institutional Review Board of the University of Illinois at Urbana-Champaign (UIUC) approved the research study, and all volunteers gave informed written consent as required by UIUC regulations and standards. The cities of Urbana-Champaign are relatively small, and the commute for most participants is generally less than 15 minutes by car. Nearly all participants drove individual cars to work.
Measures - Questionnaires
Office workers' health related quality of life was measured by Short Form 36 (SF-36), a questionnaire with 36 items related to the physical and psychosocial domains of health influenced by a person's experiences, beliefs, and perceptions of health. The SF-36 survey is a well-validated health status questionnaire that measures an individual's physical functioning, bodily pain, and perception of the ability to perform physical, social, and emotional role functions.27
The Pittsburgh Sleep Quality Index (PSQI) was utilized to evaluate subjective sleep quality of the participants. This self-rated questionnaire assesses sleep quality and disturbances over a 1-month time interval.28 The PSQI is composed of 19 self-rated questions and 5 questions rated by a bed partner or roommate. Only the self-rated items were used in scoring the scale. The 19 questions generate 7 component scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each component score ranges from 0 (no difficulty) to 3 (severe difficulty). The component scores are summed to produce a global score with a range of 0–21. A higher score indicates lower sleep quality. A PSQI global score > 5 is considered suggestive of significant sleep disturbance.
A daylight deprivation survey was administered that includes questions pertaining to demographic characteristics (age, gender, race, and working experience) and behavioral characteristics (self-reported amount of exposure to daylight on a scale of 1-10 [with 1 being always exposed and 10 being never exposed], hours of outdoor activities per day, eating behavior prior going to bed, and duration of current light exposure level).
Measures - Actigraphy
Participants wore an Actiwatch-L (Minimitter) on their non-dominant wrist. An actiwatch device is an ambulatory physiological data logger often used in research and clinical settings to detect and record motion during wake and sleep. The Actiwatch-L has an accelerometer sensitivity of 0.05 g-force and is equipped with a photodiode for measuring amount and duration of light illuminance. Participants were instructed to continuously wear these actiwatches for 2 weeks without removing them (except for bathing) during the period of time they were answering the questionnaires. Participants were also instructed to leave the actiwatches exposed to the environment at all times and to avoid covering them with clothing. The questionnaires and actiwatches were administered during late spring and summer seasons.
Valid data were recorded for a range of 6 to 10 workdays and 2 to 4 free days in participants, with the average participant yielding 8.4 workdays and 3.4 free days of actigraphy data meeting inclusion criteria for analysis, as determined by < 4 h off-wrist time per day. Analysis was conducted on Actiware software version 5 (Philips Respironics) with 30-sec sampling epochs and wake threshold value of 40 activity counts. Sleep start was defined as the first 10-min period in which no more than one epoch was scored as mobile. Sleep end was defined as the last 10-min period in which no more than one epoch was scored as immobile. Wake threshold selection was set at medium.
Actigraphy measures were calculated as the average of each participant's valid workdays (split into wake time to 08:00 for workday mornings, 08:00 to 17:00 for work hours, and 17:00 to sleep start for workday evenings) and valid free days for activity and light exposure variables, and for nighttime hours following workdays and free days for sleep variables. Actigraphy variables analyzed include total activity counts (sum of all valid physical activity counts for all epochs in the active period from wake time to 08:00 for workday mornings, 08:00 to 17:00 on workdays for work hours, 17:00 to sleep start for workday evenings, and for wake periods during free days), sleep onset time (clock time of sleep start on nights following workdays and free days), sleep onset latency (time elapsed between the start time of a given rest interval and the following sleep start time on nights following workdays and free days), sleep efficiency (the percentage of scored total sleep time to interval duration minus total invalid time for the given rest period on nights following workdays and free days), wake after sleep onset (total minutes between the start time and end time of a given sleep interval scored as wake on nights following workdays and free days), sleep time (total minutes between the start time and end time of a given interval scored as sleep on nights following workdays and free days), sleep fragmentation (sum of percent mobile and percent immobile bouts < 1 min duration to the number of immobile bouts for the given interval on nights following workdays and free days), and average light exposure (sum of all valid illuminance data in lux on a logarithmic scale for all epochs from the start time to the end time of a given interval multiplied by the epoch length in minutes from wake time to 08:00 for workday mornings, 08:00 to 17:00 on workdays for work hours, 17:00 to sleep start for workday evenings, and for wake periods during free days).
Statistical Methods
First, we performed a χ2 test (homogeneity for proportions) to compare distributions of the demographics and behavioral characteristics as measured by the daylight deprivation survey (age, race, gender, working experience, self-reported amount of exposure to daylight, hours of outdoor activities per day, eating behavior prior to going to bed, and duration of current light level exposure) between participants working in workplaces without windows and participants working in workplaces with windows. Secondly, we performed t-tests to determine any statistical difference between the two groups in terms of office workers' health related quality of life and sleep quality as measured on the SF-36 and PSQI.
For the subset of participants with actigraphy recording, distributions of the demographics and behavioral characteristics as measured by the daylight deprivation survey between workers in workplaces with no windows and workers in work-places with windows were compared to distributions in the overall group. T-tests were then utilized to gauge differences between the two groups in terms of the following previously defined actigraphy measures: total activity counts, sleep onset time, sleep onset latency, sleep efficiency, wake after sleep onset, sleep time, fragmentation index, and light exposure. Pearson bivariate correlations were run between work hour light exposure as measured by actigraphy and subjective questionnaires and other actigraphy variables.
RESULTS
Demographics and Behavioral Characteristics of the Two Groups of Workers
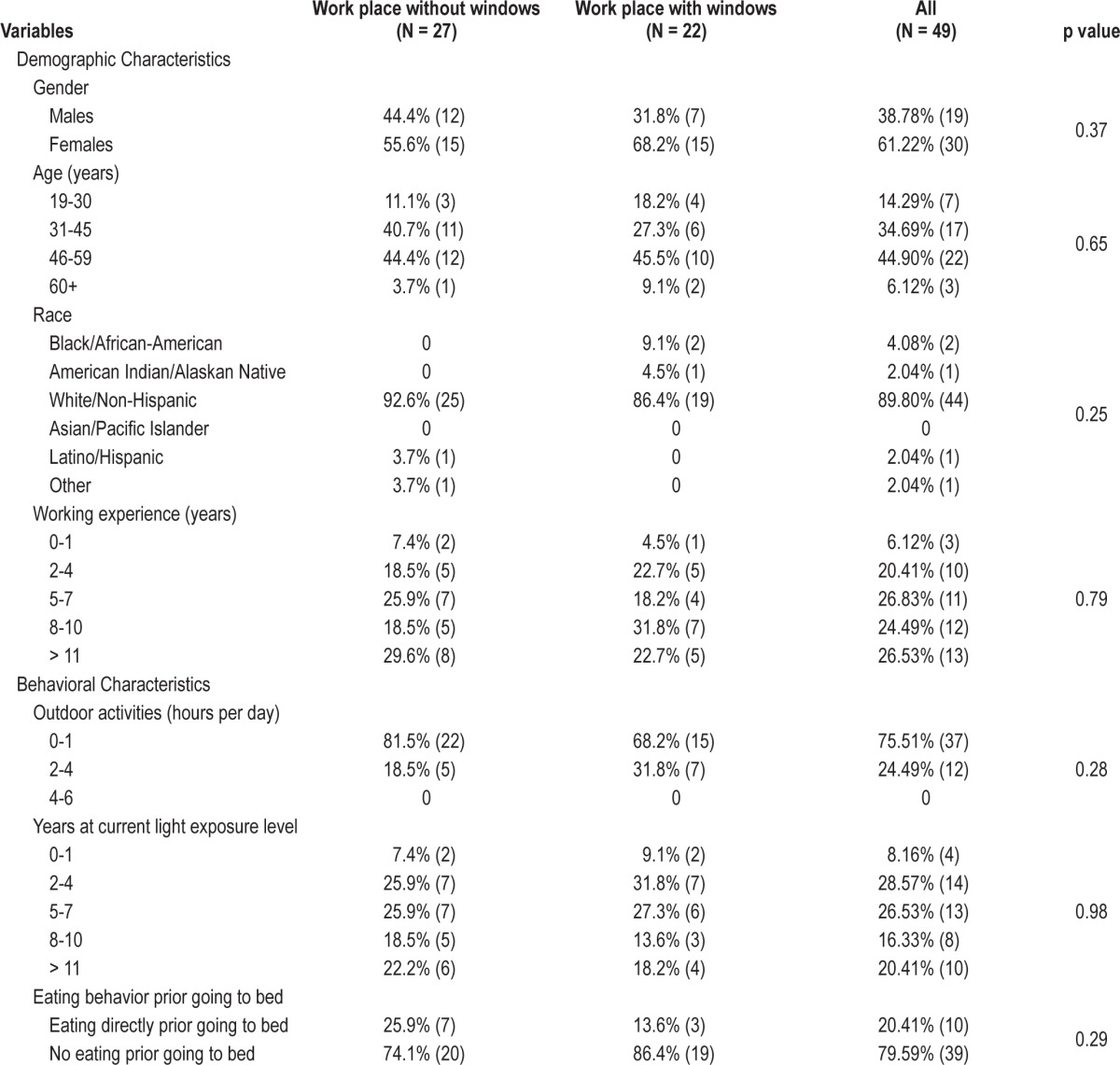
Results of the χ2 test show no significant differences between these two groups in terms of distributions of age, race, gender, working experience, hours of outdoor activities per day, eating behavior prior to going to bed, and duration of current light level exposure (Table 1). Therefore, these two groups were comparable except in their amount of self-reported amount of exposure to daylight (Table 2).
For the subset of participants with actigraphy recording, distributions of the demographic and behavioral characteristics as measured by the daylight deprivation survey between workers in workplaces with no windows and workers in work-places with windows are comparable to respective distributions in the overall group, again with no significant differences in these distributions between groups except in their amount of self-reported amount of exposure to daylight.
Light Exposure of the Two Groups of Workers
The self-reported amount of exposure to daylight scale shows office workers in workplaces without windows perceived they had significantly less exposure to daylight than office workers in workplaces with windows, as expected (Table 2). Results from actigraphy confirm average light exposure differences during work hours for the two groups, with workers in workplaces with windows receiving more light exposure than workers in workplaces without windows (Table 3 and Figure 1A; 3.00 log lux versus 2.58 log lux; p = 0.02). There was no significant difference in light exposure from wake time to start of the work period (Table 3; 2.57 log lux versus 2.38 log lux; p = 0.32); however, workers with windows in the workplace had more light exposure during workday evenings (Table 3; 2.50 log lux versus 1.93 log lux; p = 0.008) and during free days (Table 3; 3.30 log lux versus 2.37 log lux; p = 0.003) than workers without windows in the workplace. While we cannot say from our data collection whether this difference is from natural daylight or artificial lighting in the office building, workers without windows at the workplace had significantly lower average light exposure than workers with windows during workday work hours and evenings as well as during free days.

Actigraphy data collected in a subset of the office workers show that those with windows in the workplace had higher light exposure (A), more total activity (B), and longer sleep time (C) than workers without windows in the workplace. * p < 0.05, † p < 0.10.
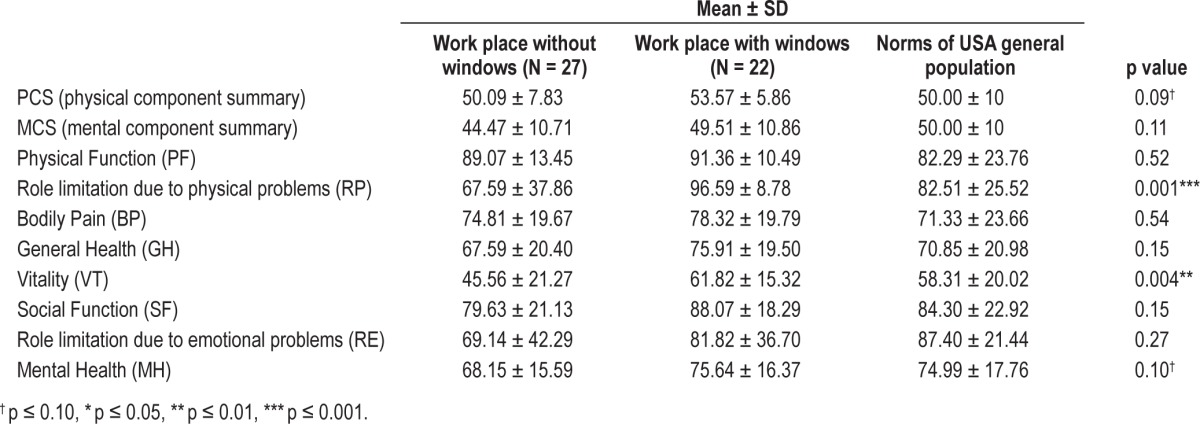
Physical and Mental Conditions of the Two Groups of Workers
Workers in workplaces without windows had significantly worse scores on two of the SF-36 dimensions—role limitation due to physical problems (RP) and vitality (VT)—than workers in workplaces with windows (Figure 2; p = 0.001 and p = 0.004, respectively). There was also a positive correlation between light exposure during work hours and role limitation due to physical problems (R = 0.503, p = 0.02). Overall, both the physical component summary (PCS) (p = 0.09) and mental component summary (MCS) (p = 0.11) scores of those in workplaces without windows were lower than scores of those working in workplaces with windows (Table 4). Participants in workplaces without windows reported poorer scores on all time on workday nights (R = 0.483, p = 0.03). While there were no significant differences between workers with windows and workers without windows in sleep onset time (21:46 versus 22:04), sleep onset latency (10 min vs 19 min), sleep efficiency (91% vs 89%), wake after sleep onset (30 min vs 37 min), and sleep fragmentation (19 vs 22) on workday nights, the averages point toward better measures of sleep quality for workers with windows at the workplace than workers without windows at the workplace during the workweek. Similarly, workers with windows at the workplace slept more than their counterparts on free day nights (506 min vs 389 min; p = 0.005), and although there were no differences in sleep onset time (22:06 vs 22:48), sleep onset latency (15 min vs 20 min), sleep efficiency (91% vs 90%), wake after sleep onset (31 min vs 36 min), and sleep fragmentation (20 vs 22) on free day nights, the averages point toward better measures of sleep quality for workers with windows at the workplace than workers without windows at the workplace during free day nights.
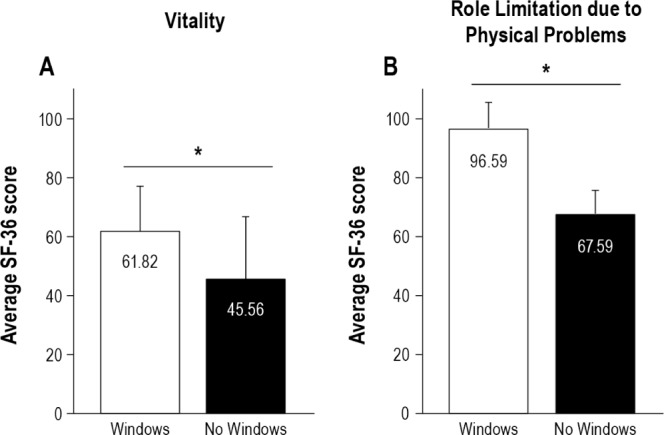
Workers with windows in the workplace reported better scores on vitality (A) and role limitation due to physical problems (B) on the SF-36 compared to workers with no windows in the workplace. * p < 0.05.
Table 5
Results of t-tests for Pittsburgh Sleep Quality Index between the two groups
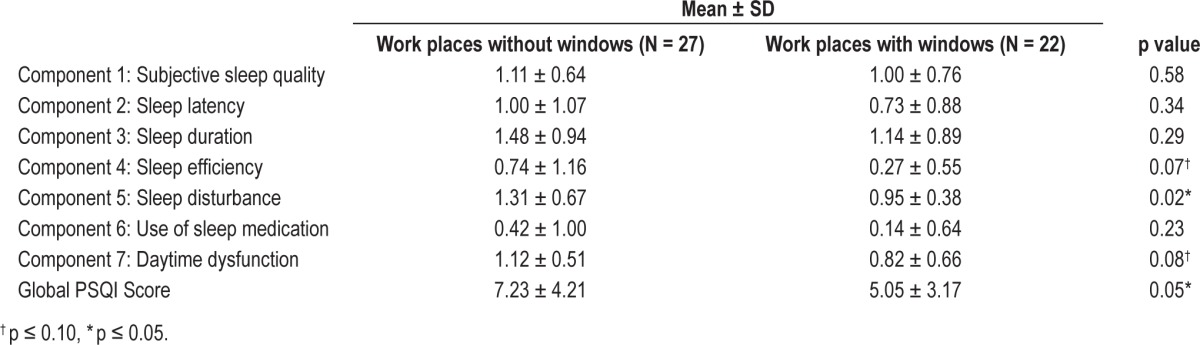
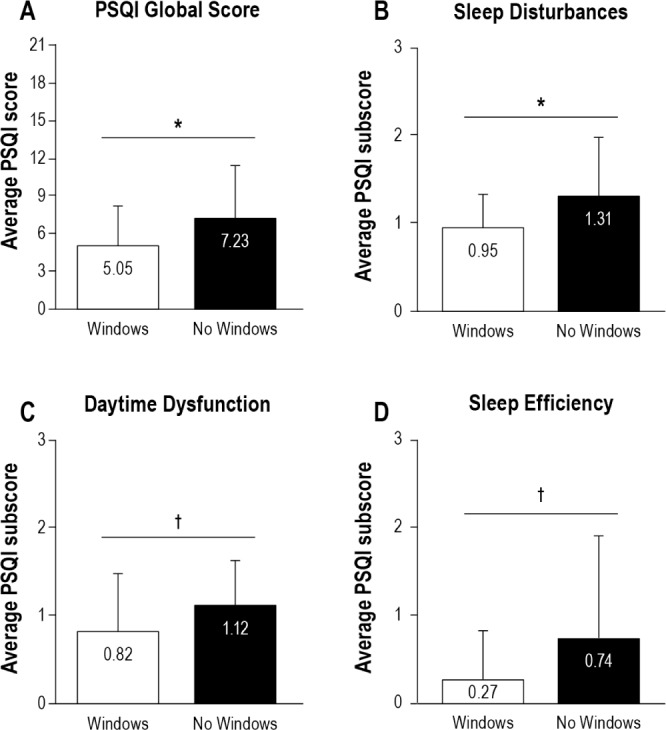
Workers with windows in the workplace reported better overall global score on the PSQI (A) compared to workers with no windows in the workplace. The difference in global score is made up mainly of differences in sleep disturbances (B), daytime dysfunction (C), and sleep efficiency (D), with workers without windows reporting poorer scores than workers with windows on all three PSQI subscores. * p < 0.05, † p < 0.10.
DISCUSSION
These results demonstrate a relationship between work-place light exposure and office workers' sleep quality, activity patterns, and quality of life. Workers in workplaces with windows not only had significantly more light exposure during work hours but also slept an average of 46 minutes more per night during the workweek than workers in workplaces without windows. Workers with windows in the workplace also had more light exposure during the workday evenings and during free days, as well as longer sleep time compared to workers without windows in the workplace. However, there were no differences in light exposure in the mornings before the work period. Workers without windows also reported poorer scores than their counterparts on the global PSQI score and the PSQI component score for sleep disturbances. None of the other component scores of the PSQI were significantly different between groups, nor were actigraphy sleep variables other than sleep time different between the groups.
These findings suggest that light exposure, or the lack thereof, during work hours may have effects beyond the workplace that impact sleep duration and quality, which may then have further effects on other health factors. Research indicates that insufficient sleep and reduced sleep quality have myriad health and safety consequences. For example, insufficient sleep and reduced sleep quality have been associated with higher evening levels of cortisol, impaired glucose metabolism, increases in appetite via decreased leptin and increased ghrelin levels, and higher body mass index, as well as increased fatigue and deterioration of performance, alertness, and mental concentration, which can lead to increased error rates and subsequent risk of injury.7–9,29–32
These health and performance consequences may affect perceived health related quality of life, as measured by the SF-36. Our results from the SF-36 show workplaces without windows have significantly negative impact on workers' role limitation due to physical problems (RP) and vitality (VT), as well as a marginal negative impact on workers' mental health compared to workplaces with windows. These results are similar to the findings of a study that examined five dimensions (GH, V, SF, RE, and MH) of the SF-36 and found that the scores of vitality (VT), social functioning (SF), and mental health (MH) for those working in dark offices are lower than scores for those working in offices with more lighting.33 Another study focusing on predictors of burnout among nurses found that exposure to at least three hours of daylight per day resulted in less stress and higher satisfaction at work.34 While those with more daylight in the workplace also have higher daily physical activity during work hours and workday evenings, our analysis cannot determine whether the workers get more activity because of the daylight or whether they have more daylight exposure due to activity. There was no difference in physical activity between the two groups during free days despite differences in light exposure during free days, and correlations between physical activity levels and light exposure during work hours, workday evenings, and free days did not suggest a strong relationship. Nonetheless, it remains a possibility that differences in activity level may influence light exposure and also sleep, yet the tendency towards higher activity levels indicates workers with more daylight exposure may have fewer physical problems or complaints regarding vitality in parallel with our findings on subjective measures of the SF-36.
Prior to this study, little was known about how architectural features such as windows impact light exposure and subsequent effects on physical and mental factors. Via examination of the influence of office settings with and without windows on office workers' light exposure, sleep, physical activity, and quality of life via actigraphy and subjective measures, this research study shows office workers in workplaces with windows may have more light exposure, better sleep quality, more physical activity, and higher quality of life ratings than office workers in work-places without windows.
This study has some limitations that could be addressed in future work. For example, the small sample size and sampling methodology could be addressed in a larger study. Participants for this study were volunteers based on a convenience sample, which may have introduced bias. The amount of light in an office may be associated with position or level of experience in the workplace; however, we found no differences in age, race, gender, years at current job, and duration of working in current light levels between workers in office settings with and without windows. We also do not have data from the participants on caffeine use, measurements of stress levels, and chronotype, which is of interest given the outcome measures of this study. Although we observed no differences in sleep onset time between the two groups of workers on workday nights and free day nights, the possibility remains that chronotype, circadian timing, or other behavioral measures may be responsible for some of the differences observed in the two groups of workers. This warrants further investigation. The objective measures of wrist actigraphy support the subjective findings; however, actigraphy data were collected for only 21 of the 49 total participants. Furthermore, although actigraphy has reasonable validity and reliability and is often used as a sleep assessment tool in sleep medicine, this methodology has some limitations. Sleep diaries were not collected in this study, and therefore were unavailable for the actigraphy analysis. For sleep-wake periods, actigraphy has low specificity for detecting wakefulness within sleep periods. Actigraphy is also neither sensitive to low light levels nor calibrated for artificial fluorescent lighting. As such, light exposure measurements for workers in office settings without windows may be an underestimate. In addition, since light exposure data are collected from the wrist, there is the possibility that error may be introduced by covering of the actiwatch, and therefore, reported values may not be fully representative of the light levels reaching the retina. Our data collection methods also do not allow for differentiation between natural daylight and artificial lighting, and do not allow for analysis of specific wavelengths of light exposure. Future studies would benefit from using devices that collect spectral distribution for comparison between the two workplace groups. Lastly, additional benefits of workplaces with windows, such as the roles of views and other dimensions, were not taken into account in this study. Views may bring some psychological dimension while daylight may have physiological effects. Future research may be able to dissociate the different roles of views and daylighting of windows. This can be done, for example, by exploring the differences between skylights that provide very limited views to the sky only versus side windows. Despite these limitations, significant differences are seen with light exposure levels and subsequent measures of sleep quality and physical and mental well-being.
As emphasized in the World Health Organization's Declaration on Occupational Health for All,1 the focal point for practical occupational health activities is the workplace. Therefore, employers have a social responsibility to plan and design a safe and healthy working environment for their employees. Some countries (such as Canada, Germany, and France) recommend certain amounts of daylight in schools and offices. Yet even in these countries it is not a requirement. In the United States, the national building code lists windows primarily as a means of emergency escape and rescue as opposed to natural lighting. Given the results of this study, we conclude that emphasizing daylight exposure and lighting in the workplace may positively affect the well-being of people working in those spaces. Lower amounts of light exposure in the workplace was associated with reduced sleep duration, poorer sleep quality, lower activity levels, and reduced quality of life in this sample of office workers. Light exposure in the workplace may therefore have long-lasting and compounding effects on the physical and mental health of the workers not only during but also beyond work hours. Enhanced indoor lighting for those with insufficient lighting in current offices as well as increased emphasis on light exposure in the architectural design of future office environments is recommended to improve office workers' sleep quality and physical well-being. Workers with limited or no access to windows in the workplace may increase their light exposure during work hours in various ways. Taking a walk during a break and enjoying lunch outdoors are simple ways to increase daytime natural light exposure. Further research is needed to determine what light exposure durations or intensities are sufficient or optimal for benefits to well-being.
DISCLOSURE STATEMENT
This was not an industry supported study. This research was supported by the Illinois Campus Research Board of the University of Illinois at Urbana-Champaign and NIH grants 5T32 HL790915 and P01 AG11412. Dr. Zee has a Philips/Respironics Educational/Research Gift to Northwestern University, owns stock in Teva, and is a consultant for Sanofi-Aventis, UCB, Johnson and Johnson, Merck and Co, Takeda, Purdue, Philips, Jazz, Vanda, and Ferring. Dr. Reid has received research support from Philips Consumer Lifestyles for research unrelated to the work reported in the paper. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Drs. Boubekri and Cheung contributed equally to this work. The authors thank the subjects for their participation.