Reckless Self-destructive Behavior and PTSD in Veterans: The Mediating Role of New Adverse Events
Abstract
The addition of self-destructive and reckless behavior as a symptom of posttraumatic stress disorder (PTSD) in DSM-5 has stimulated renewed interest in understanding relationships between these behaviors and trauma-related psychopathology. This study examined the relationship between reckless and self-destructive behaviors (RSDB), intervening exposure to new adverse events, and later PTSD severity in a sample of trauma-exposed veterans. At baseline, participants were assessed for RSDB (past 5 years) and current PTSD severity (N = 222). PTSD severity was then reassessed approximately 4 years later (N = 148). Overall, RSDB were reported by 74.4% of the sample, with 61.3% engaging in multiple forms of RSDB. The most commonly endorsed behaviors included alcohol/drug abuse (42.8%), driving while intoxicated (29.4%), gambling (24.7%), and aggression (23.1%). RSDB correlated positively with PTSD severity at both the baseline (r = .16, p = .031) and follow-up assessment (r = .24, p = .005). Path models indicated that exposure to new adverse events fully mediated the effect of Time 1 RSDB on PTSD symptoms at Time 2 (indirect association: β = .05, p =.046). Results suggest that RSDB are common among trauma-exposed veterans and may perpetuate PTSD symptoms by increasing exposure to new adverse events.
Military personnel engage in reckless and self-destructive behaviors (RSDB) including substance abuse, self-harm, excessive gambling, and aggression more frequently than their civilian counterparts (Killgore et al., 2008; Thomsen, Stander, McWhorter, Rabenhorst, & Milner, 2011). These behaviors pose a serious public health burden, as illustrated by recent findings indicating that the risk of suicide is 41-61% higher for veterans than civilians (Kang et al., 2015), and that veterans are more frequently incarcerated for violent offenses than non-veterans (Berzofsky, Bronson, Cason, & Noonan, 2015). Given the significant social and financial costs associated with RSDB, more research is needed to better understand how these behaviors impact the health and wellbeing of veterans. Moreover, the addition of the “reckless and self-destructive behavior” symptom in the DSM-5 PTSD diagnosis highlights the importance of understanding the interplay of RSDB and PTSD.
According to the National Institutes of Health (2013), excessive alcohol consumption occurs at much higher rates among military personnel than civilians, with 47% of all active duty service members reporting binge drinking. Veterans also have a lifetime prevalence of pathological gambling that is two times higher than the general population (Westermeyer et al., 2013). Other RSDB found to be elevated in veterans include reckless driving leading to fatal motor vehicle crashes (Hooper et al., 2006), aggression in those with PTSD (Jakupcak et al., 2007), and self-harm behavior (Kang et al., 2015). Notably, one study found that active duty personnel who report one risky behavior are at significantly higher risk for other types of risky behavior, suggesting that these behaviors frequently co-occur and may share etiological mechanisms (Thomsen et al., 2011).
Previous cross-sectional studies have found that PTSD and deployment-related stressors are associated with increased engagement in RSDB (Kelley et al., 2012; Killgore et al., 2008; James et al., 2014). For example, James et al. (2014) found that PTSD among veterans was associated with more frequent risky, impulsive, and suicidal behavior, regardless of the co-occurrence of traumatic brain injury. Based on these and other findings, RSDB was recently added as a symptom of PTSD. While it is possible that RSDB are best conceptualized as a symptomatic correlate of PTSD, it is also conceivable that they serve to maintain or exacerbate the condition by putting individuals at risk for exposure to additional traumas and/or new adverse events. Driving while intoxicated, for example, increases the likelihood of experiencing a traumatic motor vehicle accident, overt aggression can elicit assaultive behavior from others, and drug use can increase exposure to drug-related crime and physical injury. Considering that as many as one-third of patients with PTSD develop a chronic form of the condition that persists for years (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995) and a substantial proportion report reckless behavior (e.g., James et al., 2014), clarifying the influence of these behaviors on the symptom course could shed light on a previously under-recognized factor that contributes to the maintenance of chronic PTSD.
This study examined RSDB and their relationships with PTSD severity in a sample of veterans with a high prevalence of PTSD. We focused on understanding the relationship of RSDB with PTSD (rather than other psychiatric disorders), because our sample was recruited based on a probable PTSD diagnosis. We hypothesized that the majority of participants would endorse RSDB based on Thomsen et al. (2011) who found that over half of active duty personnel reported some type of risky behavior. We also examined the relationship between RSDB and PTSD symptoms over time, which was an extension of a previous study conducted in this sample that examined reciprocal relationships between PTSD and normal range personality traits (Sadeh, Miller, Wolf, & Harkness, 2015). In that study, we found that trait negative emotionality and disconstraint (i.e., impulsivity) indirectly influenced later PTSD symptoms by increasing exposure to new adverse events. In the current study, we examined the specific influence of RSDB on change in PTSD severity over time and the mediating influence of new onset adverse life events.
Specifically, using path analysis we tested the following competing hypotheses (see Figure 1): (1) RSDB directly influences later PTSD severity (direct effects only model); or alternatively, (2) RSDB influences PTSD symptom course, in whole or in part, by increasing exposure to new adverse events. That is, (2a) if exposure to new adverse events fully mediates the association between RSDB and PTSD symptoms, then we expected to find significant direct paths from RSDB to new events and from new events to future PTSD symptoms, but no direct path from RSDB to future PTSD symptoms On the other hand, (2b) if new adverse events only partially mediate the association between RSDB and PTSD, then we expected to observe both direct paths from RSDB to future PTSD and indirect associations through new event exposure. We included the personality traits that we previously linked to new onset adverse events as covariates in these models to evaluate the specificity of the effects of RSDB on PTSD.
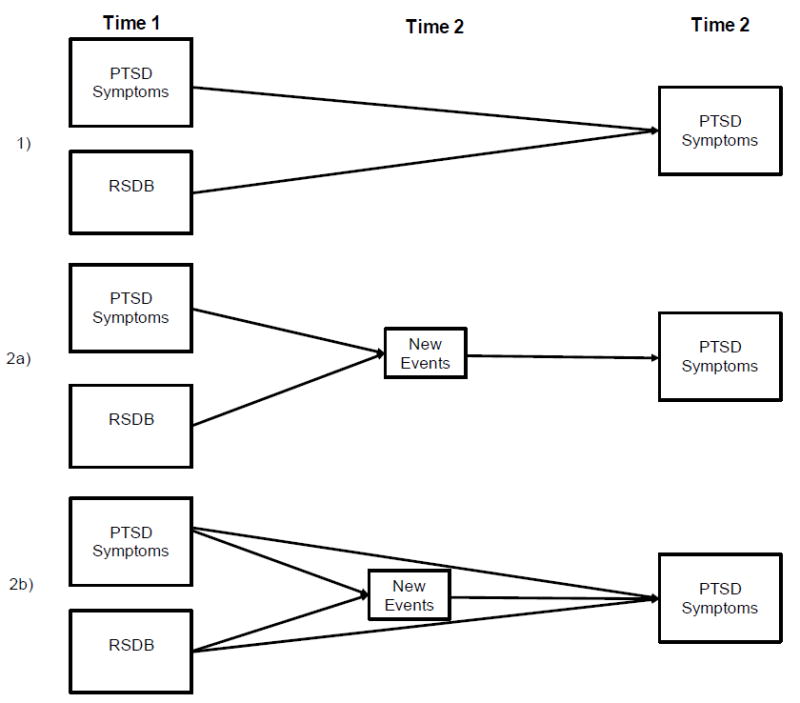
Competing hypotheses regarding the influence of RSDB on later PTSD severity. (1) Direct paths only: RSDB directly influences later PTSD. (2a) Exposure to new adverse events fully mediates the association between RSDB and T2 PTSD. (2b) New adverse events only partially mediates the association between RSDB and T2 PTSD.
Methods
Participants
We recruited 242 veterans from VA Boston Healthcare System who screened positive for probable DSM-IV PTSD (at least one B symptom, three C symptoms, and two D symptoms) during a telephone screen using the PTSD Checklist-civilian version (PCL-C; Weathers, Litz, Herman, Huska, & Keane, 1993). Twenty participants were excluded due to incomplete data, not meeting inclusion criteria upon further assessment, or withdrawing from the study.
The final sample consisted of 222 veterans aged 23 to 68 (M = 50.83, SD = 10.73), who were mostly men (n = 201, 90.5%). Participants self-identified as White (n = 175, 78.8%), Black/African-American (n = 43, 19.4%), and/or American Indian or Alaskan Native (n = 15, 6.8%). Eight (3.6%) endorsed Hispanic/Latino ethnicity, seven (3.2%) indicated racial origin was unknown, and 27 (11.5%) did not provide ethnicity information. The majority of participants were unemployed or receiving disability payments (n = 142, 63.9%), followed by full or part time employment (n = 53, 23.9%), retired (n = 20, 9.0%), students (n = 3, 1.4%), or did not indicate employment (n = 4, 1.8%). Participants served during the Vietnam War (n = 124, 55.9%), OEF/OIF (n = 32, 14.4%), Operation Desert Storm (n = 24, 10.8%), and the Korean War (n = 2, 0.9%). Forty-seven participants (21.2%) endorsed “other service eras” and 0.9% did not indicate service era.
Participants completed an initial assessment (T1) and a follow-up assessment (T2) approximately 4 years later (M = 3.9, SD = 0.81; Range = 2.45-6.13), and 148 of the original 222 participants returned for T2 (66.7% response rate). There were no statistically significant differences between individuals with follow-up data versus those without on T1 PTSD severity, PTSD diagnosis, gender, income, or any race/ethnicity category (smallest p ≥ .191). Individuals who did not complete T2 endorsed more RSDB, t(192) = 1.28, p = .023, than participants who completed both assessments.
Measures
RSDB
At T1, a clinical psychologist or graduate-level psychology trainee administered the International Personality Disorder Examination (IPDE; Loranger, 1995), a standardized 99-item interview. We focused on questions that assessed different forms of RSDB: sexual impulsivity (#63), irritability and aggressiveness (#71), reckless driving (e.g., driving while intoxicated; #73), excessive gambling (#76a), excessive abuse of drugs and alcohol that led to functional impairment (#76b), eating binges (#76c), failure to plan ahead (#69), and self-harm (#77). Responses to these questions were coded from videotaped interviews on a 0-2 scale by trained research technicians: 0 = denied or not supported by the participant description, 1 = occasionally engaged in the behavior, and 2 = frequently engaged in the behavior. Behaviors that were currently endorsed or endorsed in the five years prior to the T1 assessment were coded. A composite RSDB variable was created by summing across items (Cronbach’s alpha coefficient = .72). To be included in the analysis, participants must have had usable data for the majority of items on the IPDE (28 were excluded for missing >2 responses). For participants with missing items but usable data, the total score was pro-rated using the available items. Participants missing IPDE data were excluded from the descriptive statistics and correlational analyses but included in the path models.
PTSD
Participants were assessed at each time point using the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1990), a 30-item diagnostic interview designed to assess the frequency and intensity of the 17 DSM-IV PTSD criteria on a 5-point scale. The index trauma was combat for 101 (45.5%) participants, actual or threatened physical assault for 34 (15.3%) participants, childhood sexual trauma for 19 (8.6%) participants, sudden death of a friend/loved one for 17 (7.7%) participants, accident for 15 (6.8%) participants, and adult sexual trauma for 10 (5.0%) participants. Each of the other index traumas (e.g., life threatening illness, stalked) was endorsed by less than 4.0% of the sample. Although all participants screened positive for probable PTSD with the PCL-C on the initial phone screening, only 55% met criteria for PTSD on the CAPS at the in-person T1 assessment, and 57% met criteria for PTSD at T2. CAPS scores spanned a range of severity (T1: Min/Max = 3/123; T2: Min/Max = 0/110). Inter-rater reliability based on secondary ratings of videotaped interviews for approximately one-third of participants was high (intraclass correlation coefficient = .93 for both time points).
New Adverse Events
At T2, participants were asked whether events from the Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000) had occurred since the date of their initial assessment. We did not assess whether the events met full criteria for the DSM-IV definition of trauma and consequently refer to them as adverse events rather than traumatic events. Our interest was in events whose occurrence could plausibly be influenced by engagement in RSDB. That is, we only included events where RSDB had the potential to increase or decrease exposure to such events, even if other individual difference factors (e.g., personality traits, mental health symptoms, socioeconomic resources) may have also influenced exposure to that event. As such, we excluded the natural disaster item of the TLEQ, because exposure to this type of event is almost entirely outside an individual’s control, making it unlikely that engagement in RSDB would influence exposure to it. A count variable was created by summing the different types of events endorsed during the follow-up period from the following list: motor vehicle accident, combat, sudden death of friend/loved one, life-threatening/disabling event to loved one, life-threatening illness, robbery or assaulted with a weapon, assaulted by an acquaintance or stranger, witnessed severe assault to an acquaintance or stranger, threatened with death or serious harm, unwanted sexual contact, sexual harassment, stalked, miscarriage, abortion.
Personality Traits
At T1, participants completed the Multidimensional Personality Questionnaire-Brief Form (MPQ-BF; Patrick, Curtin, & Tellegen, 2002) to assess personality traits. The MPQ-BF consists of 155 items (11 primary trait scales, 12 items each) that contribute to three higher-order temperament scales assessing negative emotionality (NEM), positive emotionality (PEM), and constraint (CON). NEM refers to an individual’s tendency towards negative emotions, aggression, and hostility (i.e., Stress Reaction, Alienation, and Aggression scales); PEM refers to an individual’s tendency towards positive emotions, sociability, and social dominance (i.e., Social Potency, Wellbeing, Achievement, and Social Closeness scales); and CON assesses impulsivity (reversed), thrill-seeking (reversed), and social conformity (i.e., Control, Harm Avoidance, and Traditionalism scales). NEM, PEM, and CON were created by summing weighted raw scores of the primary scales that make up each higher-order temperament scale (Patrick, Curtin, & Tellegen, 2002). The MPQ-BF has a mostly true to mostly false response format.
Procedure
Participants were recruited for T1 through flyers posted around the hospital, clinician referrals, and a database of veteran research volunteers. All participants completed a consent form to be contacted for future research, which was used to contact participants for T2. The study was not originally designed to be longitudinal, which contributed to attrition at T2. VA Boston Healthcare System Institutional Review Board and Research and Development Committees approved the study prior to data collection. Participants gave written informed consent after research assistants provided them with a detailed description of the study. Doctoral- and masters-level clinical psychologists and clinical psychology trainees conducted the interviews, which typically lasted three to four hours. Participants received $15-$20/hour.
Data Analysis
Analyses were conducted using SPSS version 22 (Armonk, NY: IBM Corp.) and Mplus 7.11 (Muthén & Muthén, 2013). Based on previous work (Allison, 2003), we used robust maximum likelihood estimation, which accounts for missingness using full-information maximum likelihood (FIML) estimation that uses all available data (e.g., participants with any T1 data) and accounts for non-normality of variables. This is superior to listwise deletion and imputation (Allison, 2003), because it represents the variance in scores at T1, whereas eliminating subjects based on the completion of both time points would likely lead to biased parameter estimates due to differences in those who did and did not complete T2. The maximum percentage of missing data was 36.5% across variables. The final sample size was 120/148 for the descriptive statistics and correlational analyses with/and without RSDB in the analysis. For the path analysis, the final sample size was 222 and included all participants with any available T1 data.
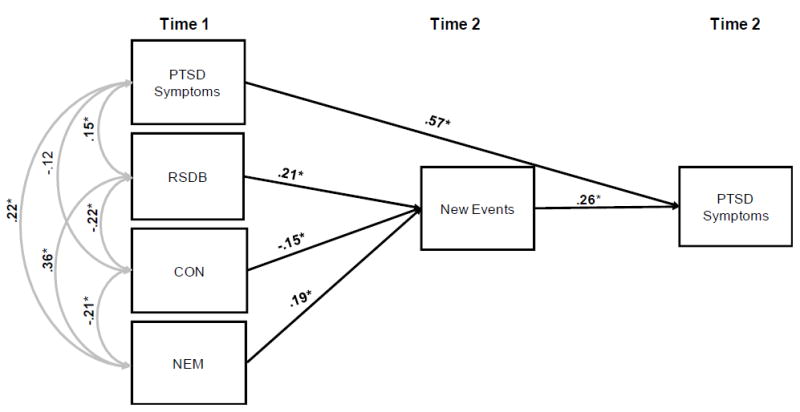
Temporal relationships between RSDB and PTSD were examined in a series of path analyses. First, we specified a fully saturated model (Figure 2) with all direct paths and indirect associations, which served as the base model for comparisons with the nested models. In subsequent analyses, we compared models that examined direct effects only (i.e., whether RSDB directly influenced future PTSD), indirect effects only (i.e., whether RSDB influenced PTSD indirectly via exposure to new events), and hybrid models against the fully saturated model. Model fit was evaluated by comparing overall model chi-square (small and non-significant values indicate good model fit) and standard cut-off scores for good model fit (Hu & Bentler, 1999), specifically, root mean square error of approximation (RMSEA < .06), standardized root mean square residual (SRMR < .08), confirmatory fit index (CFI ≥ .95), and Tucker-Lewis index (TLI ≥ .95). We also compared models using the Akaike information criterion (AIC; Akaike, 1987), with lower values preferred over higher values. The fit of nested models was compared using a chi-square difference testing approach that adjusted for the scaling correction factor employed with robust maximum likelihood estimation (Satorra & Bentler, 2001). Indirect effects were evaluated using Model INDIRECT. We included NEM and CON in the model to show that the current findings cannot be accounted for by these variables, given the similarities between this study and Sadeh et al. (2015). Using the rule-of-thumb of 5:1 for the ratio of sample size to free parameters (Bentler & Chou, 1987) produced a minimum required sample size of 135. Thus, our sample of 222 was adequate for the current analyses.
Results
Overall, 74.4% of the sample reported past 5-year RSDB, with 61.3% engaging in multiple forms of RSDB. The most commonly endorsed RSDB were alcohol and drug abuse (42.8%), driving while intoxicated (29.4%), gambling (24.7%), and aggression (23.1%). Between T1 and T2, 82% of the sample reported at least one new adverse event, and the mean number reported was 1.86 (SD = 1.96, range: 0-9). The most commonly reported adverse events were sudden death of a friend or loved one (36.5%), threatened with or completed physical assault (24.3%), motor vehicle accident (22.3%), life-threatening or disabling event to a loved one (20.3%), life-threatening illness (19.6%), and witnessing a severe accident (8.1%).1
Estimated means, standard deviations, and bivariate correlations are listed in Table 1. As hypothesized, RSDB correlated positively with T1 and T2 PTSD severity. It also correlated positively with new adverse events during the follow-up period, consistent with the possibility that these behaviors increase exposure to stressful events. Bivariate relations with the personality variables showed that RSDB, T1/T2 PTSD severity, and new adverse events were all positively associated with NEM, whereas RSDB and new adverse events were inversely correlated with CON.1
Table 1
Descriptive Statistics and Bivariate Correlations.
| Variable | M (SD) or N (%) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|
| Time 1 | |||||||||
| 1 RSDB (M, SD) | 2.11 (2.1) | ||||||||
| 2 PTSD symptoms (M, SD) | 53.7 (25.4) | .16* | |||||||
| 3 Age (M, SD) | 50.8 (10.7) | -.38** | -.22* | ||||||
| 4 Male sex (N, %) | 201 (90.5) | -.11 | -.09 | ||||||
| 5 Negative emotionality (M, SD) | 54.7 (18.1) | .37** | .22* | -.08 | -.11 | ||||
| 6 Positive emotionality (M, SD) | 50.9 (16.9) | .04 | -.23* | -.17* | -.05 | -.07 | |||
| 7 Constraint (M, SD) | 77.3 (13.3) | -.22* | -.12 | .15* | -.08 | -.21* | -.01 | ||
|
| |||||||||
| Time 2 | |||||||||
| 8 PTSD symptoms (M, SD) | 53.5 (25.9) | .24* | .58** | -.15 | -.01 | .28* | -.16 | .13 | |
| 9 New major adverse events (M, SD) | 1.9 (2.0) | .28* | .03 | -.12 | -.04 | .29* | .03 | -.22* | .28* |
Note.
Sex: 0 = female; 1 = male. Time 1: N = 222; Time 2: N = 148.
Path analysis
First, we examined whether RSDB directly influenced later PTSD severity or whether it influenced it indirectly via exposure to new adverse events (Table 2). To test these hypotheses, we compared models using a nested design. The fully saturated model (Figure 2) that included all direct paths and indirect associations served as the base model for comparisons with the nested models. We included direct paths from T1 personality traits (NEM and CON) to the T2 variables (new event exposure and PTSD) to ensure that the results could not be accounted for by these associations based on previous work (Sadeh et al., 2015). Direct paths from T1 RSDB to new events (p = .025), new events to T2 PTSD (p = .006), and T1 PTSD to T2 PTSD (p < .001) were all significant in the fully saturated model. The paths from T1 NEM (p = .049) and CON (p = .034) were significant predictors of new events, but they did not predict T2 PTSD [NEM: p = .151; CON: p = .812]. The direct path from T1 PTSD to new events was not significant (p = .643; as reported in Sadeh et al., 2015) nor was the direct path from RSDB to T2 PTSD (p = .305).
Table 2
Model Fit Indices and Model Comparisons.
| X2 | df | RMSEA | SRMR | CFI | AIC | TLI | Model Comparison | ΔX2 (Δ df) | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Saturated model | 0.00 | 0 | 0.00 | 0.00 | 1.00 | 8572.19 | 1.00 | ||
| 2. Direct paths only | 24.05 | 5 | 0.13 | 0.11 | 0.75 | 8589.65 | 0.55 | Model 2 vs. 1 | 24.05(5)* |
| 3. Indirect associations only | 55.74 | 4 | 0.24 | 0.12 | 0.32 | 8632.28 | -0.52 | Model 3 vs. 1 | 55.74(4)* |
| 4. Final model | 4.09 | 4 | 0.01 | 0.03 | 0.99 | 8568.75 | 0.99 | Model 4 vs. 1 | 4.09(4) |
Note. df = degrees of freedom. RMSEA = root mean square error of approximation. SRMR = standardized root mean square residual. CFI = confirmatory fit index. AIC = Akaike information criterion. TLI = Tucker-Lewis index.
Next, we tested the hypothesis that T1 RSDB only directly influences T2 PTSD (controlling for T1 PTSD) by setting the indirect effects from the full model to zero. Setting the indirect associations to zero significantly degraded model fit compared to the base model (ΔX2 = 24.05, Δ df = 5, p < .001). Then, we tested the hypothesis that RSDB only indirectly influences future PTSD severity via exposure to new events (controlling for T1 PTSD effects on new event exposure) by setting the direct effects from the base model to zero. This indirect effects only model was also rejected, because it significantly damaged fit relative to the fully saturated model (ΔX2 = 55.74, Δ df = 4, p < .001).
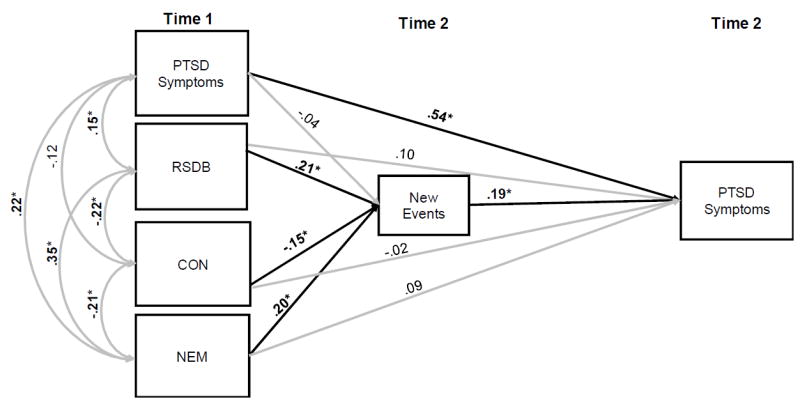
Finally, we tested a hybrid model by setting non-significant paths in the fully saturated model (Figure 2) to zero. This model permitted a test of the hypothesis that T1 RSDB influences T2 PTSD indirectly via new event exposure, and that T1 PTSD influences T2 PTSD directly. Examination of the fit indices indicated that this final model provided good fit to the data and did not degrade model fit relative to the fully saturated model (ΔX2 = 4.09, Δdf = 4, p = .393). Standardized parameter estimates are provided in Figure 3. The direct path from RSDB to new events was significant (p = .027), indicating that higher levels of RSDB predicted increased exposure to future adverse events. The direct path from new events to T2 PTSD was also significant (p < .001), suggesting that new adverse events during the follow-up period increased PTSD symptoms at T2. The autoregressive path from T1 to T2 PTSD was also significant (p < .001). As hypothesized, the indirect path from T1 RSDB to T2 PTSD via new events was significant (β = .05, SE = .03, p = .046) when controlling for T1 PTSD. This finding suggests that new event exposure mediated the relationship between T1 RSDB and T2 PTSD. The model explained 41% of the variance in T2 PTSD.2
Final Model. RSDB = Reckless Self-Destructive Behaviors. PTSD = Posttraumatic Stress Disorder. New Events = Intervening adverse events assessed at T2. NEM = Negative Emotionality. CON = Constraint. *p< .05.
In summary, the path analyses showed that exposure to new adverse events fully mediated the relationship between T1 RSDB and T2 PTSD, controlling for the influence of T1 PTSD. However, new event exposure did not mediate the relationship between T1 PTSD and T2 PTSD, suggesting that RSDB and PTSD influence subsequent PTSD severity in different ways.
Discussion
Although RSDB have long been known to co-occur with PTSD and are now included in the DSM-5 definition of the disorder, relatively little is known about how these behaviors might impact trajectories of chronic PTSD. Thus, the goal of this study was to assess RSDB in a sample of trauma-exposed veterans with a high prevalence of PTSD and examine how these behaviors influence the course of PTSD. At Time 1, almost three-fourths of the sample reported RSDB in the last five years, and 61.3% of participants had engaged in two or more of these behaviors. RSDB at baseline was associated with higher future PTSD symptoms, and exposure to new adverse events during the follow-up period mediated this relationship.
The most prevalent RSDB reported in the sample were alcohol/drug abuse and driving while intoxicated, with 42.8% and 29.4% of the sample endorsing these behaviors, respectively. According to a national epidemiological study, almost half (46.4%) of individuals diagnosed with PTSD also meet criteria for substance abuse (Pietrzak, Goldstein, Southewick, & Grant, 2011). This high comorbidity may reflect individuals with PTSD abusing alcohol and drugs as a method to cope with symptoms (Chilcoat & Breslau, 1998) or shared risk factors across these disorders (e.g., a propensity towards impulsivity and thrill seeking; Miller et al., 2006). The third most prevalent RSDB was aggression, endorsed by 23.1% of the sample, which converges with prior work suggesting that people with PTSD are more likely to be aggressive than those without (Jakupcak et al., 2007). Moreover, Elbogen et al. (2014) found that OEF/OIF veterans with PTSD were at an increased risk of engaging in severe violence and physical aggression compared to those without PTSD. Although we did not perform a comprehensive analysis of pre-trauma factors that might be influencing rates of RSDB in this sample, the association of these behaviors with trait negative emotionality and disconstraint suggests that these personality traits are likely contributors.
We also tested the hypothesis that RSDB influences the course of PTSD by increasing exposure to new adverse events. The best-fitting model included significant direct paths from RSDB to new event exposure and from new event exposure to future PTSD. Further, mediation analyses indicated that the indirect effect from RSDB to future PTSD via new event exposure was significant and necessary for overall model fit. Thus, results suggest that RSDB increases exposure to new adverse events, and this exposure mediates the relationship of RSDB with future PTSD severity. Based on the types of stressful events endorsed during the follow-up period, our findings may reflect the tendency for individuals who engage in RSDB to select into dangerous environments that put them at risk for physical injury (e.g., car accidents, assaultive events) and/or associate with others who place themselves at risk for premature death or life-threatening injury (e.g., aggressive or substance-abusing individuals). This finding converges with our previous study (Sadeh et al., 2015), which found that the personality traits of negative emotionality and disconstraint perpetuate PTSD symptoms over time, in part, by increasing exposure to new adverse events. However, a key difference between this study and Sadeh et al. (2015) is that, here, we examined behaviors that are typically considered dangerous and pathological (e.g., drug abuse, aggression) and thus may be of greater interest to clinicians.
One clinical implication of our finding that RSDB contributes to the maintenance of PTSD symptoms is of the need to focus greater assessment and treatment efforts on these problems in trauma-exposed groups. The addition of the reckless/self-destructive behavior symptom to the DSM-5 PTSD diagnosis can facilitate screening for RSDB in clinical settings and potentially flag behaviors that put veterans at risk for future trauma and chronic PTSD trajectories. Our results also suggest that augmenting trauma-specific interventions with treatments to target RSDB may be beneficial for veterans whose continued exposure to adverse events is perpetuating posttraumatic symptomatology. Future research on the reciprocal influences of PTSD and RSDB over time, aimed at identifying mediators of these associations (e.g., emotional dysregulation, poor cognitive control), could point to new targets for intervention.
Notably, we found that RSDB was associated with future PTSD severity solely through exposure to subsequent stressors, whereas other PTSD symptoms were not. These findings suggest that RSDB and PTSD influence subsequent PTSD severity in different ways, and RSDB may not be a core symptom of the disorder. Rather, RSDB may have a causal (albeit indirect) impact on the course of PTSD, which could explain their frequent comorbidity. This interpretation has been suggested by some recent research showing that the reckless/self-destructive symptom does not load particularly well on the DSM-5 PTSD hyperarousal factor (Miller et al., 2013). Although the inclusion of RSDB as a symptom of PTSD can stimulate research on relationships between these constructs and raise awareness of their frequent co-occurrence, current results call into question the recent diagnostic revision and suggest that more research is needed to evaluate the validity of RSDB as a symptom of PTSD.
Study conclusions should be weighed in light of several limitations. First, this study was not originally designed to assess RSDB or prospective relationships between RSDB and PTSD. Consequently, RSDB items were extracted post-hoc from a structured personality disorder interview, and data were not collected on the presence of RSDB prior to trauma exposure, military deployment, or PTSD onset. These design limitations precluded examining whether RSDB influenced the onset or chronicity of PTSD, whether RSDB worsened after PTSD onset, and trajectories of RSDB in individuals prior to joining the military, during active duty, and/or post deployment. Thus, longitudinal research that uses measures specifically designed to assess reckless/ self-destructive behavior and examines the interplay of RSDB, trauma exposure, military history, and PTSD over time is needed before stronger conclusions about directionality among these factors can be made. Second, given that participants were recruited from a VA facility, and many were unemployed or disabled, our sample is likely not representative of all veterans with PTSD. Our sample also spanned diverse war eras and endorsed high rates of multiple trauma types. Given that we were unable to assess these variables in our model, the impact of mental health treatment, specific trauma types – especially combat exposure, and time since deployment on RSDB-PTSD relationships requires further study. Third, the extent to which the findings generalize to other populations, especially civilian women, remains untested. Fourth, in constructing the final hybrid model, we used a data-driven approach that relied on significant p-values from previously tested models, which can potentially bias the results in moderate sample sizes. Thus, replication of these findings in an independent sample will be important. Finally, although this study focused on the relationship between RSDB and PTSD, it is possible that similar associations would be observed with diagnoses other than PTSD (e.g., substance use or mood disorders). Future studies may benefit from approaching RSDB as a transdiagnostic phenomenon, given its relevance to multiple disorders.
Despite these limitations, the study had several strengths, including a longitudinal design and recruitment of a clinically-relevant sample of trauma-exposed veterans. It also benefited from clinical diagnostic interviews to assess PTSD and RSDB. Considering the number of veterans who have been diagnosed with PTSD and are reintegrating into society, understanding how reckless behaviors relate to the maintenance of PTSD symptoms is an important area of study. This study found high rates of RSDB among trauma-exposed veterans, and results are consistent with the possibility that engagement in these harmful behaviors perpetuates PTSD symptoms over time.
Acknowledgments
Funding for this study was provided by a Department of Veterans Affairs, Clinical Science Research and Development Program award 5I01CX000431-02 awarded to M.W. Miller and a Career Development Award to E.J. Wolf from the Department of Veterans Affairs, Clinical Sciences Research and Development Program.
Footnotes
1These data overlap with the results found in Sadeh, Miller, Wolf, & Harkness (2015).
2Due to item overlap in the measurement of RSDB and PTSD with regard to aggressive behavior, we reran all analyses after removing the irritable and aggressive behavior symptom from the total PTSD score. Removing this symptom did not change the results substantially or produce new findings.
Views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of Veterans Affairs.
References
- Akaike H. Factor analysis and the AIC. Psychometrika. 1987;52(3):17–332. doi: 10.1007/BF02294359. [CrossRef] [Google Scholar]
- Allison PD. Missing data techniques for structural equation modeling: Structural equation modeling. Journal of Abnormal Psychology. 2003;112(4):545–557. http://dx.doi.org/10.1037/0021-843X.112.4.545. [PubMed] [Google Scholar]
- Bentler PM, Chou CP. Practical issues in structural modeling. Sociological Methods & Research. 1987;16(1):78–117. doi: 10.1177/0049124187016001004. [CrossRef] [Google Scholar]
- Berzofsky M, Bronson J, Carson A, Noonan M. Veterans in prison and jail 2011-2012. Bureau of Justice Statistic 2015 [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. Behavior Therapist. 1990;13(8):187–188. [Google Scholar]
- Chilcoat HD, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addictive behaviors. 1998;23(6):827–840. doi: 10.1016/S0306-4603(98)00069-0. [PubMed] [CrossRef] [Google Scholar]
- Elbogen EB, Johnson SC, Wagner HR, Sullivan C, Taft CT, Beckham JC. Violent behaviour and post-traumatic stress disorder in US Iraq and Afghanistan veterans. The British Journal of Psychiatry. 2014;204(5):368–375. doi: 10.1192/bjp.bp.113.134627. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Hooper TI, DeBakey SF, Bellis KS, Kang HK, Cowan DN, Lincoln AE, Gackstetter GD. Understanding the effect of deployment on the risk of fatal motor vehicle crashes: a nested case–control study of fatalities in Gulf War era veterans, 1991–1995. Accident Analysis & Prevention. 2006;38(3):518–525. doi: 10.1016/j.aap.2005.11.009. [PubMed] [CrossRef] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [CrossRef] [Google Scholar]
- Jakupcak M, Conybeare D, Phelps L, Hunt S, Holmes HA, Felker B, McFall ME, et al. Anger, hostility, and aggression among Iraq and Afghanistan war veterans reporting PTSD and subthreshold PTSD. Journal of Traumatic Stress. 2007;20(6):945–954. doi: 10.1002/jts.20258. [PubMed] [CrossRef] [Google Scholar]
- James LM, Strom TQ, Leskela J. Risk-taking behaviors and impulsivity among veterans with and without PTSD and mild TBI. Military Medicine. 2014;179(4):357–363. http://dx.doi.org/10.7205/MILMED-D-13-00241. [PubMed] [Google Scholar]
- Kang HK, Bullman TA, Smolenski DJ, Skopp NA, Gahm GA, Reger MA. Suicide risk among 1.3 million veterans who were on active duty during the Iraq and Afghanistan wars. Annals of Epidemiology. 2015;25(2):96–100. doi: 10.1016/j.annepidem.2014.11.020. [PubMed] [CrossRef] [Google Scholar]
- Kelley AM, Athy JR, Cho TH, Erickson B, King M, Cruz P. Risk propensity and health risk behaviors in US army soldiers with and without psychological disturbances across the deployment cycle. Journal of Psychiatric Research. 2012;46(5):582–589. doi: 10.1016/j.jpsychires.2012.01.017. [PubMed] [CrossRef] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [PubMed] [CrossRef] [Google Scholar]
- Killgore WD, Cotting DI, Thomas JL, Cox AL, McGurk D, Vo AH, Hoge CW. Post-combat invincibility: Violent combat experiences are associated with increased risk-taking propensity following deployment. Journal of Psychiatric Research. 2008;42(13):1112–1121. doi: 10.1016/j.jpsychires.2008.01.001. [PubMed] [CrossRef] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12(2):210–224. http://dx.doi.org/10.1037/1040-3590.12.2.210. [PubMed] [Google Scholar]
- Loranger A, Janca A, Sartorius N. International Personality Disorders Examination (IPDE) Geneva. Switzerland: World Health Organization; 1995. [Google Scholar]
- Miller MW, Greif JL, Smith AA. Multidimensional Personality Questionnaire profiles of veterans with traumatic combat exposure: Internalizing and externalizing subtypes. Psychological Assessment. 2003;15:205–215. http://dx.doi.org/10.1037/1040-3590.15.2.205. [PubMed] [Google Scholar]
- Miller MW, Vogt DS, Mozley SL, Kaloupek DG, Kean TM. PTSD and Substance-Related Problems: The mediating roles of disconstraint and negative emotionality. Journal of Abnormal Psychology. 2006;115:369–379. http://dx.doi.org/10.1037/0021-843X.115.2.369. [PubMed] [Google Scholar]
- Miller MW, Wolf EJ, Kilpatrick D, Resnick H, Marx BP, Holowka DW, Friedman MJ. The prevalence and latent structure of proposed DSM-5 posttraumatic stress disorder symptoms in US national and veteran samples. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5(6):501. http://dx.doi.org/10.1037/a0029730. [Google Scholar]
- Muthén LK, Muthén BO. Mplus 7.11. Los Angeles, CA: Muthén & Muthén; 2013. [Google Scholar]
- National Institute of Health. Drug facts: Substance abuse in the military. National Institute on Drugs Abuse: The Science of Drug Abuse and Addiction. 2013 Retrieved from: https://www.drugabuse.gov/publications/drugfacts/substance-abuse-in-military.
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychological Assessment. 2002;14(2):150–163. http://dx.doi.org/10.1037/1040-3590.14.2.150. [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders. 2011;25:456–465. doi: 10.1016/j.janxdis.2010.11.010. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Sadeh N, Miller MW, Wolf EJ, Harkness KL. Negative emotionality and disconstraint influence PTSD symptom course via exposure to new major adverse life events. Journal of Anxiety Disorders. 2015;31:20–27. doi: 10.1016/j.janxdis.2015.01.003. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66(4):507–514. doi: 10.1007/BF02296192. [CrossRef] [Google Scholar]
- Thomsen CJ, Stander VA, McWhorter SK, Rabenhorst MM, Milner JS. Effects of combat deployment on risky and self-destructive behavior among active duty military personnel. Journal of Psychiatric Research. 2011;45(10):1321–1331. doi: 10.1016/j.jpsychires.2011.04.003. [PubMed] [CrossRef] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124–133. http://dx.doi.org/10.1037/1040-3590.11.2.124. [Google Scholar]
- Westermeyer J, Canive J, Thuras P, Oakes M, Spring M. Pathological and Problem Gambling among Veterans in Clinical Care: Prevalence, Demography, and Clinical Correlates. The American Journal on Addictions. 2013;22(3):218–225. doi: 10.1111/j.1521-0391.2012.12011.x. [PubMed] [CrossRef] [Google Scholar]


 Facebook
Facebook
 Twitter
Twitter
 Google+
Google+